Immunization was introduced to the world in 1798, by Dr. Edward Jenner against the smallpox virus and was a major milestone in modern Medicine.
Regardless of the centuries of research saving generations of humankind against preventable, if not lethal, and majorly debilitating bacterial and viral infections like poliomyelitis, wherein Sri Lanka the virologically confirmed Poliomyelitis patient was last reported in 1993, why is there still a group referred to as “anti-vaxxers” and parental refusers with controversies against vaccinations.
Vaccine refusal is mainly based on religious and philosophical beliefs, safety concerns, and common questions preferably answered by a healthcare professional.
Here we will address the latter to eliminate “Vaccine hesitancy”.
1. What is the EPI schedule?
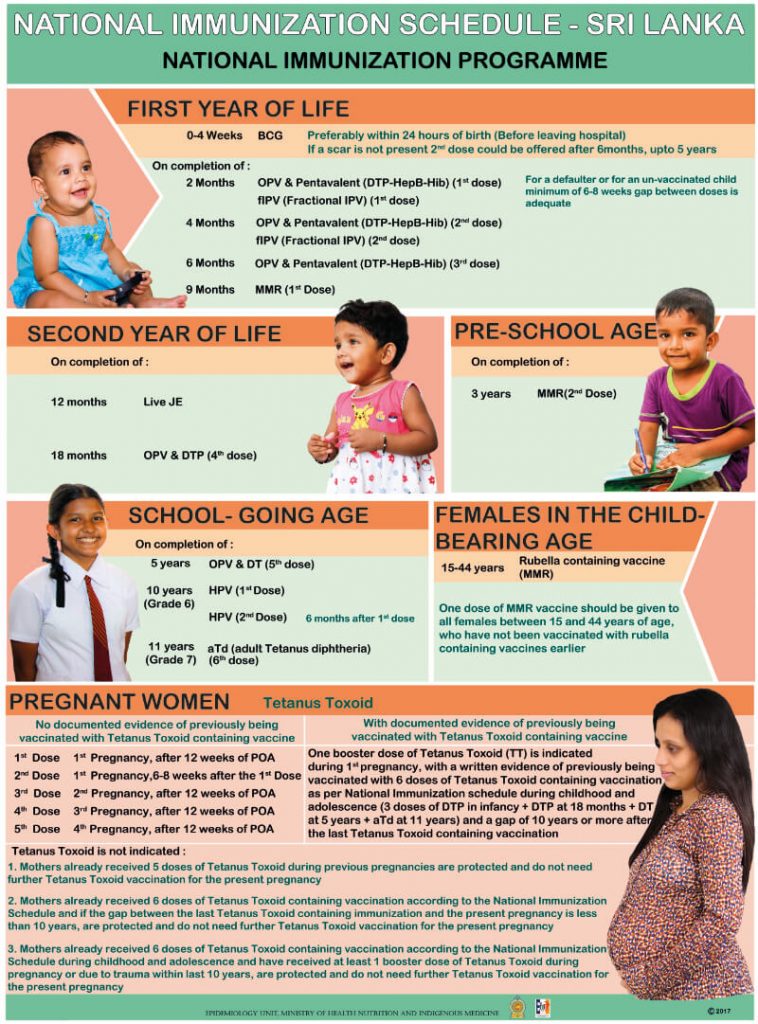
Sri Lankans currently adhere to the Expanded Program of Immunization (the EPI) introduced by the WHO and UNICEF as early as 1886.The schedule is reviewed frequently based on the latest scientific data and made thorough over the last two decades ensuring high immunization coverage and disease control.
2. How are vaccines timed on the schedule?
This is based on;
- The age when the body’s immune system can develop optimum post-vaccine immunity.
- Providing protection as early as possible to the vulnerable age groups.
Certain vaccines may need more than 1 dose to top up the “antibody titer” for complete results. These are repeated at research-based intervals.
Ex; The OPV (oral polio vaccine) is administered to infants at 2, 4, and 6 months and boosted at 18 months and 5 years.
(Please refer to the detailed National Immunization Schedule, Sri Lanka below)
3. What are contraindications for immunization?
The EPI schedule is applicable under ideal conditions but there may be certain exceptions.
A few absolute contraindications are;
- Severe acute illness like a viral infection with fever (The vaccine can be delayed a few days until such a condition settles and the interval for the next dose can be calculated accordingly)
- A state of severe immunodeficiency like Leukemia
- Progressive neurological disorders
- Children with severe brain malformations have a risk of developing post-vaccine seizures and Encephalitis. For example, the pentavalent vaccine is avoided in children with West syndrome.
- But a common myth is to avoid vaccines like Japanese Encephalitis for children with epilepsy. These children can be administered the vaccines in a special setup with emergency care access if they have been seizure-free for 1 year.
- Known allergies to vaccine or vaccine components
Some relative contraindications are,
- Live vaccines are avoided in pregnancy
- Immunosuppressive states like in HIV/AIDS and patients with malignancy receiving chemotherapy.
A minor cough or cold, history of Bronchial Asthma, prematurity, family history of fits, treatment with antibiotics or low dose steroids, chronic heart or lung diseases are not reasons to avoid vaccines.
4. Should multiple shots in one visit be avoided?
Certain vaccines in the EPI are given collectively. Eg; at 2 months, the OPV is given with the Pentavalent vaccine (DPT, Hep B, and Hib) This concerns certain parents that they are overwhelming the child’s immune system.
But children generally are exposed to thousands of germs every day while eating, drinking, playing, and even breathing. They are continuously producing hundreds of antibodies naturally!
5. What to expect post-vaccine?
Commonly children develop minor reactions like fever and soreness over the injection site, especially for the live-attenuated vaccines like MMR which can be managed with acetaminophen and hydration for the 1st 48 hours.
A severe allergic reaction, indicated by trouble breathing, hives, sweating, and swelling of the face or throat, is very rare but will need immediate medical attention.
6. Why vaccinate if getting the disease gives you natural immunity?
Most vaccine-preventable diseases have lethal and permanent complications. Ex. Childhood mumps infection in a male child can get complicated as mumps-orchitis causes infertility in adulthood.
The basis of the vaccine is to introduce the body to an altered, unharmful version of a pathogen, where you don’t get the disease but develop immunity against the disease.
Immunization aims for artificially induced immunity as prevention is better than cure. Over the years they have significantly reduced morbidity and mortality in regard to vaccine-preventable diseases.
Sri Lanka’s immunization program is widely recognized as one of the most consistent and effectively controlled health programs in South Asia and is one of the best in the world. The EPI is available in any MOH for free with island-wide coverage.
Therefore, nothing should stop you from getting you or your child immunized unless advised otherwise by a medical professional for absolutely medical reasons only!
Please see the National Immunization Schedule of Sri Lanka below.